Rescue Robbie Prototype
Endovascular Resusctation Simulator
From previous design iterations and in-depth insights from the HEMS teams at the London Air Ambulance (LAA) there has been a need identified to create a higher fidelity training manikin. In developing the EVAC device a high fidelity but portable and realistic simulator will be essential for training users to perform this rare but high stakes and high stress procedure and for regular practice to keep initial training and skills topped up. The simulator concept and design is such that it does not require prolonged set up and is simple use for to the simulation lead. Thus it can be used for short but high yield training sessions which make it ideal for running sims, for example in between clinical cases or during short training windows.
It is also designed to be robust, portable and simple to trouble shoot with a balance between high fidelity, reliable mechanics and user friendly interface so that it may be used in ‘real life’ pre- hospital situations i.e. under a heavy goods vehicle or in a cramped hallway, out in the wind and rain, in all temperatures etc. This will hugely improve the realism of simulations and therefore the cognitive yield from training scenarios, as compared to high tech but stationary ‘lab table’ or ‘sim suite’ type models such as those in current existence.
Despite it’s portability it is able to accurately reproduce a model of exsanguination (controllable by the operator), a realistic response to complete and partial REBOA (with variations akin to human physiology, depending on site, timing and degree of balloon inflation, site and size of vascular injury and concomitant resuscitation of the mannequin).
Existing trainers for these procedures are separate and therefore do not support trainee decision making. The ROB Manakin provides freedom
in response to a simulated accident, therefore making training scenarios more realistic. The current training set up at London’s Air Ambulance is dictated by the availability of numerous devices which simulate different procedures. This leads to the team practicing ‘procedures’ (such as REBOA, thoracotomy or central venous access) rather
than ‘situations’ (such as rapid exsanguination) and deviates from real life clinical practice in these emergencies.
This mannequin aims to have the capability
to simulate all key procedures required for resuscitating a patient who is exsanguinating, extremely shocked or in traumatic cardiac arrest. These procedures include Thoracotomy, REBOA (both by the percutaneous and open surgical cut down route), central venous access through which the mannequin may be resuscitated with volume (bringing with it physiologically appropriate changes in blood pressure above and below the balloon and flow beyond it, if a balloon is in situ).
The mannequin may also be set to bleed from zones 1, 2 or 3 (or any combination of these) at variable rates so that the team must act accordingly (both in speed and in type/site of intervention to resuscitate the patient and choose from the various resuscitative options available to them. We believe this will bring far more realistic training, both in
the procedures themselves and. Critically, to the decision making required in these time pressured situations. This will be particularly useful in learning when and how to deploy the EVAC device, as well as interpreting the response to it, in amongst the resuscitation of a critically injured patient.
The aim of this project is to develop a novel training manikin for London’s Air Ambulance.
By adapting an existing manikin with bespoke modules, trainees will be able to practise any of the following procedures:
• Resuscitative endovascular balloon occlusion of the aorta (REBOA)
• Resuscitative Extracorporeal Membrane Oxygenation (ECMO) and ECMO CPR
• Resuscitative thoracotomy (RT)
• Surgical cutdown (SC)
• Subclavian vein catheterisation (SVC)
In developing the EVAC device a high fidelity but portable and realistic simulator will be essential for training users to perform this rare but high stakes and high stress procedure and for regular practice to keep initial training and skills topped up. The simulator concept and design is such that it does not require prolonged set up and is simple use for to the simulation lead. Thus it can be used for short but high yield training sessions which make it ideal for running sims, for example in between clinical cases or during short training windows.
It is also designed to be robust, portable and simple to trouble shoot with a balance between high fidelity, reliable mechanics and user friendly interface so that it may be used in ‘real life’ pre- hospital situations i.e. under a heavy goods vehicle or in a cramped hallway, out in the wind and rain, in all temperatures etc. This will hugely improve the realism of simulations and therefore the cognitive yield from training scenarios, as compared to high tech but stationary ‘lab table’ or ‘sim suite’ type models such as those in current existence.
Despite it’s portability it is able to accurately reproduce a model of exsanguination (controllable by the operator), a realistic response to complete and partial REBOA (with variations akin to human physiology, depending on site, timing and degree of balloon inflation, site and size of vascular injury and concomitant resuscitation of the mannequin).
The team for this project
The day to day team for creating the training manikin are:
Dr S. Sadek – LAA
He is acting as the main touch point for the specific design needs of the training manikin and the research into how it may be used in the training scenarios.
Dr S. Scott - ECMO Consultant
Responsible for endovascular task trainers, thermoplastic modeling and ECMO compatability.
R. Holland – F31 BV
F31 is a design and innovation agency based out of the Netherlands, Rich has over 25yrs of experience (13yrs in London, 10yrs in Sweden). F31 are acting as the administrative conduit for the design development and working more with technical aspects of the training manikin.
Dr. M. de Haas – Master Digital Design
Based out of the Amsterdam University of Applied Sciences the course focusing on designing and innovation around digital and physical interaction design with about 50/60 students.
Existing trainers for these procedures are separate and therefore do not support trainee decision making. The MAPS Trainer (working title) provides freedom in response to a simulated accident, therefore making training scenarios more realistic.
An additional factor is the cost of manikin adaptation. It is our aim to develop a reasonably low cost model whilst maintaining a high level
of fidelity. Therefore many of our design solution prototypes have been created in a “DIY” fashion.
Since the project is REBOA-focused, funds have primarily been used developing flesh modules hitherto and a battery based circulatory system with zone based bleed out valves. This has included purchase and trialling of several possible materials, alongside manufacturing unique vessel structures to replicate the anatomy to a far higher degree than LAA’s previous models.
Part of the process to date has been to attend the BIG SICK 2022, were we gave a sucessful demostration of the training manakin.
Additional components, for the other
procedures, have also been purchased for research and development purposes. A brief summary of these stages can be found on the following pages..
Following completion of the REBOA and SC modules, focus can now be transferred to the thoracic cage. This section houses both the RT and SVC modules. An example of an existing RT model can be found here, with no cost available, and an SVC model can be found here, costing $1,899.
It is our goal to create modules and a
training manikin that provide realism on
par with these models at far lower expense.
This will make the training system more accessible to a wider target group.
Summary of finalised parts
REBOA + surgical cut-down modules
• Manikin based simulator
• Ultrasound compatible medical grade
gelatin, three distinct layers, with housing. • Bespoke tubing arrangement for
replicating vessels.
Fluid circuit
• Bleed-out valves with electronic control to simulate zonal bleeding.
• Fluid reservoir and collection system. • Pressure montior.
• Manual pulse feedback.
• Fluid circuit and control system..
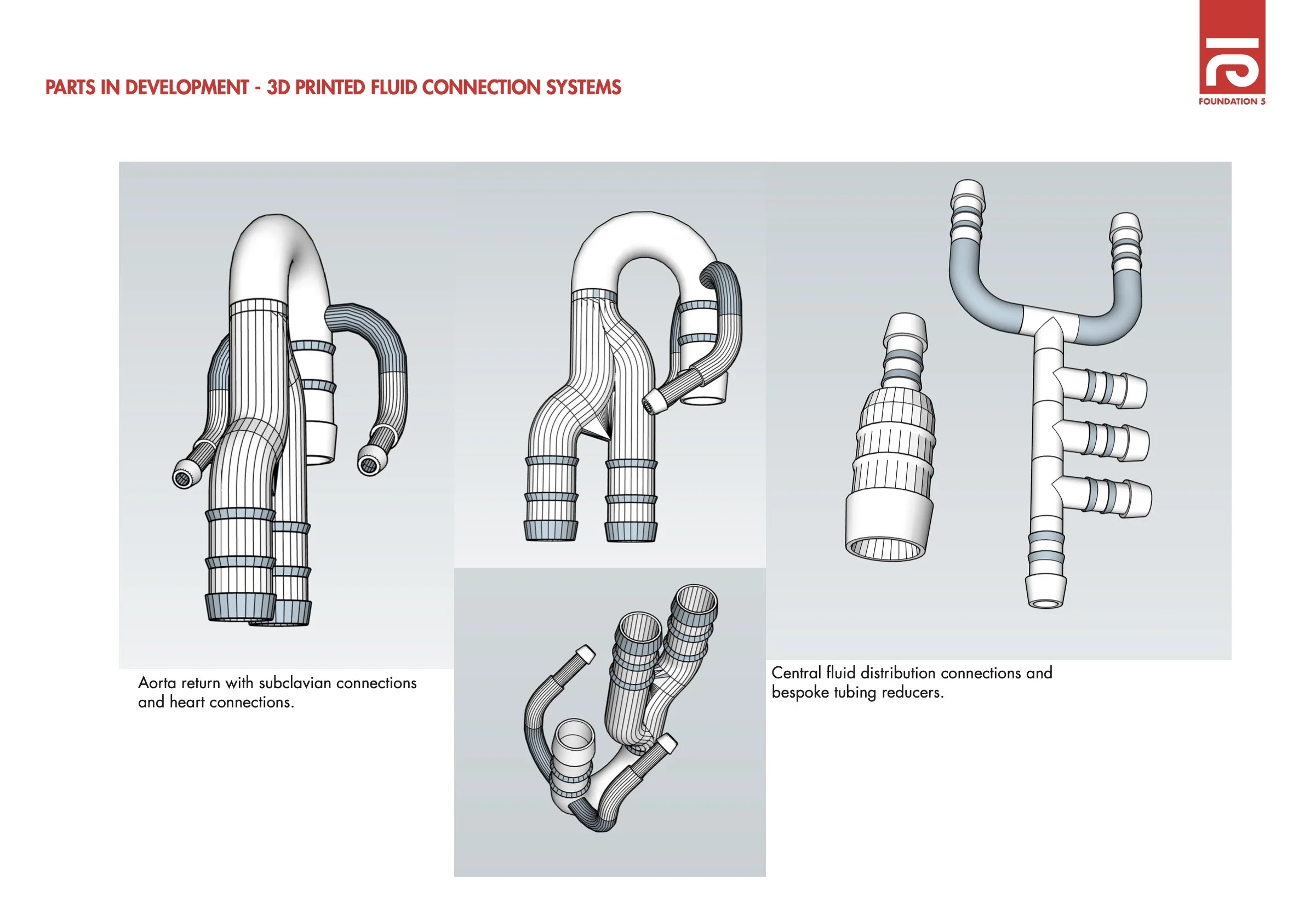
ARTS BREAKDOWN
To further develop ROB, the funding needs to be broken down in relation to the various parts that are already in development, and or to be developed further.
Some of the parts to be developed may need a lot more in-depth study due to the complexity of them. However, a lot can be created intially from a DIY perspective and then fine turned later on.
PARTS DEVELOPED IN MK1
Resuscitative thoracotomy module.
Some research is needed to get the
parts right, and some need developing, but to add a higher fidelity to the existing manakin would need the following:
Subclavian vein catheterisation module
• This can be modeled and 3D printed
• Parts of this can be 3D printed, the self sealing gel would be part of the gel blocks
Fluid circuit
• 3D Heart that can pump.
• Precise system pressure creation. • 3D printed manifolds & system. • Different bleed out speeds.
TO DEVELOP MK2 FOR 18/19 APRIL
Heart model
Improving heart model and it’s pump function (e.g. 3D printed heart and major vessels with integral valves for better ‘manual internal CPR’ function.
Realism
Improved realism in the case of thoracotomy for other interventions such as release of tamponade, repair of cardiac wounds and cardiac vascular access.
Elastic
Developing elastic major vascular tree akin to true anatomical vascular properties.
Gel Blocks
Better gel blocks: replacing the latex tubing and ballistics gel with a self sealing material ‘tract closing’ material in order to improve usability and reducing turnover and cost of disposables thereby reducing long term costs and improving practicality.
Real ROB
A more realistic ROB, the better the fidelity of the sim and the effects on human factors / non technical skills.
Pressure monitoring
Realistic pressure indicator on control pannel and injection site.
TO FURTHER DEVELOP MK3
Shock
Simulate the true picture of shock due to wound in major vessel (broader pulse pressures and result- ant pump failure), the resultant cardiac failure and simulate (plus potentially study) the effect of aortic occlusion on this pathology.
AI
Simulate the effects of haemorrhage, arterial holes, REBOA and volume resuscitation on the flows and pressures the simulator generates in order to further improve fidelity beyond mechanical responses.
RC
Wireless control and monitoring.
ECMO
Ability to apply the same mannequin to pre-hospital ECMO (currently being trialed by LAA) for both ‘medical’ cardiac arrest and traumatic cardiac arrest. As discussed with HEMS PHC ECMO leads and is greatly desired, no such simulator which
is both high fidelity and portable is in use for true pre-hospital environment scenarios.
EPR & SAAP
Ability to be used for EPR and SAAP,
both concepts which are being explored
as future avenues for pre-hospital endovascular resuscitation by LAA thereby expanding its appli- cation even more and future proofing the simulator and it’s value to us.